Understanding Cavities in Mouth: What You Need to Know
Cavities in mouth are damaged areas in your teeth that develop into tiny holes or openings. They’re also called tooth decay or dental caries. Here’s what you need to know:
Quick Facts:
- What they are: Holes in teeth caused by bacteria and acid
- How common: Over 80% of Americans have at least one cavity by their mid-30s
- Main causes: Bacteria, sugar, poor oral hygiene, and acid attacks on tooth enamel
- Symptoms: Toothache, sensitivity to hot/cold/sweet foods, visible holes or dark spots
- Treatment: Fluoride treatments, fillings, crowns, or root canals depending on severity
- Prevention: Brush twice daily with fluoride toothpaste, floss, limit sugar, visit your dentist regularly
Cavities are one of the most common chronic diseases affecting people of all ages. Nearly all adults aged 65 or older have had a cavity at some point in their lives. Half of children aged 6 to 9 have experienced at least one cavity in their baby or permanent teeth.
The good news? Tooth decay is largely preventable. Understanding how cavities form and what you can do to stop them is the first step toward protecting your smile and your overall health.
I’m Dr. Shawn Casey, founder of Casey Dental, and I’ve been treating cavities in mouth and helping families maintain healthy smiles in northeast Pennsylvania since 1994. My practice focuses on using modern technology and preventive care to help patients avoid tooth decay before it starts.
What Causes Cavities in Mouth and How Do They Form?

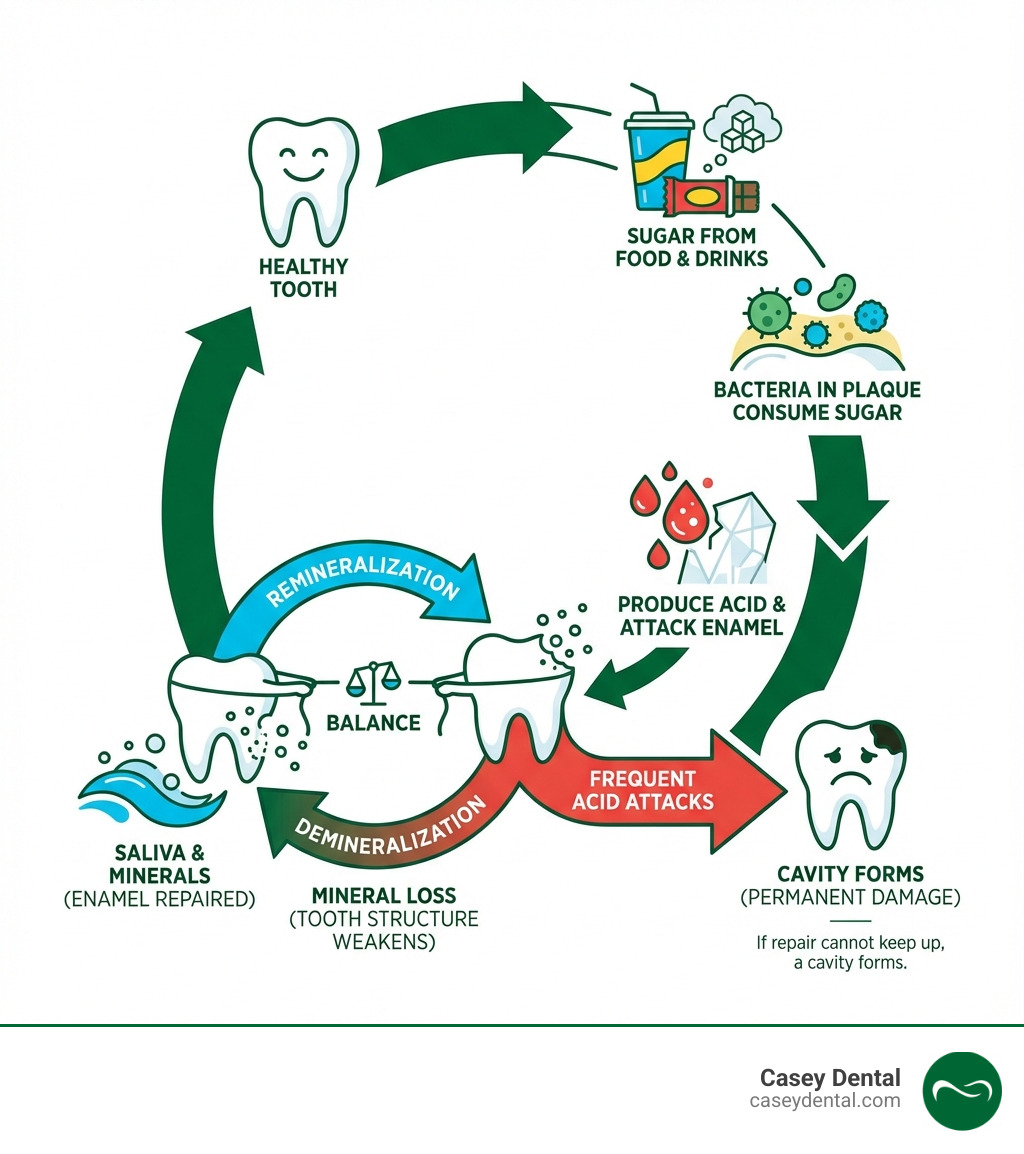
At its core, a cavity in mouth is a hole in your tooth resulting from tooth decay. This process is a daily “tug-of-war” in our mouths between damaging factors (bacteria, sugar, acid) and protective ones (saliva, fluoride). Harmful bacteria in our mouths feed on sugars and starches from food, producing acids that attack the tooth’s hard outer layer, the enamel. This attack is called demineralization.
These bacteria, along with food particles and saliva, form a sticky film on our teeth called plaque. Plaque protects the bacteria as they continue producing acid, which slowly eats away at the enamel.
Fortunately, our saliva plays a crucial protective role. It contains minerals like calcium and phosphate that help neutralize these acids and repair the enamel in a process called remineralization. However, if acid attacks are too frequent or oral hygiene is poor, our teeth can’t repair themselves fast enough. The enamel weakens until a permanent hole—a cavity—forms, which requires dental repair.
For more in-depth information on this fascinating battle, you can read more about tooth decay and cavities.
The Main Causes and Risk Factors
While the basic process is straightforward, several factors increase your risk for developing cavities in mouth:
- Poor Oral Hygiene: Not brushing and flossing properly allows plaque to build up, creating a haven for acid-producing bacteria.
- Frequent Snacking and Sipping: Constantly eating or drinking sugary/starchy items exposes teeth to repeated acid attacks, preventing enamel from recovering.
- Sugary and Acidic Drinks: Sodas, juices, and sports drinks bathe teeth in sugar and acid, speeding up decay.
- Dry Mouth (Xerostomia): Reduced saliva from medical conditions or medications lowers your natural defense against acid, significantly increasing cavity risk.
- Insufficient Fluoride Exposure: Not enough fluoride from water or toothpaste leaves teeth vulnerable, as fluoride strengthens enamel and aids repair.
- Worn Fillings or Dental Devices: Old fillings or ill-fitting appliances can trap food and bacteria, making cleaning difficult and promoting decay.
- Eating Disorders & Acid Reflux: Conditions like bulimia or GERD expose teeth to strong stomach acids, causing severe enamel erosion.
- Genetics: Some people are naturally more prone to cavities due to softer enamel or specific oral bacteria.
- Age: Children (developing habits) and older adults (receding gums, dry mouth) are often at higher risk.
- Parental Transmission of Bacteria: Cavity-causing bacteria can be passed from parent to child through sharing utensils or kissing.
Understanding these risk factors allows us to take proactive steps to protect our smiles. For a more detailed look at the causes, you can explore this cavity overview from Casey Dental.
How Diet Contributes to Cavities in Mouth
Our diet plays an enormous role in developing cavities in mouth. It’s not just what we eat, but how often we eat it.
- Sugar’s Role in Feeding Bacteria: Harmful mouth bacteria feed on sugars and starches from snacks, candy, and refined carbs. This produces the acid that starts tooth decay.
- Acidic Foods and Drinks Eroding Enamel: Items like citrus fruits, sodas, and sports drinks directly erode enamel, weakening teeth and making them more susceptible to decay.
- Sticky Foods: Foods like caramel or chips cling to teeth, prolonging sugar exposure and giving bacteria more time to produce acid.
- Constant Sipping and Snacking: Frequency matters more than quantity. Each sip or bite starts a ~20-minute acid attack. Frequent snacking keeps teeth under constant assault, preventing natural repair.
- Importance of Water: Drinking water, especially after meals, rinses away food particles and sugar. It also stimulates saliva, which neutralizes acid and helps repair enamel.
Limiting fruit juice intake is important for protecting teeth at any age.
The Stages and Symptoms of Tooth Decay

Understanding the progression of cavities in mouth is crucial for simpler, less invasive treatment. Tooth decay is a gradual, five-stage process. The good news is that early-stage decay is reversible, which is why regular dental check-ups are so important for catching problems when they’re small.
For more general oral health information, the Mouth Healthy website is a fantastic resource.
Stage 1-2: Early Decay and Symptoms
- Stage 1: White Spots (Demineralization): The first sign of decay is a white, chalky spot where enamel has lost minerals from acid attacks. There is no hole or pain yet, and this stage is reversible with good hygiene and fluoride, which helps the enamel remineralize.
- Stage 2: Enamel Decay: If demineralization continues, the enamel breaks down and a small cavity begins to form. It’s often painless and may only be spotted by a dentist during an exam.
It’s important to distinguish between a cavity and a tooth stain. While both can appear as dark spots, they are very different:
| Feature | Cavity (Tooth Decay) | Tooth Stain |
|---|---|---|
| Appearance | Can be white, brown, black; often a distinct pit/hole | Usually brown, yellow, or grey; flat discoloration |
| Texture | Soft, sticky, or rough when probed by a dentist | Smooth; does not feel rough or soft |
| Location | Often in pits/grooves, between teeth, or near gum line | Can be anywhere, often on smooth surfaces or near gum line |
| Progression | Will worsen over time if untreated | Cosmetic; does not damage tooth structure; can be polished off |
| Symptoms | Pain, sensitivity (in later stages) | No pain or sensitivity |
| Reversibility | Only in earliest ‘white spot’ stage | Often removable with professional cleaning or whitening |
Stage 3-5: Advanced Decay and Long-Term Consequences
If early decay isn’t treated, it will progress deeper into the tooth, leading to more significant damage and noticeable symptoms.
- Stage 3: Dentin Decay: Decay reaches the softer dentin layer under the enamel. Since dentin has tubules leading to the nerve, you’ll likely feel sensitivity to hot, cold, or sweet things.
- Stage 4: Pulp Involvement: Decay reaches the tooth’s innermost pulp (nerves and blood vessels). This causes a significant toothache, spontaneous pain, or pain when biting, indicating inflammation or infection.
- Stage 5: Abscess Formation: In the most severe stage, an untreated pulp infection spreads to the bone, forming a painful pocket of pus (an abscess). Symptoms include severe, throbbing pain, facial swelling, and fever.
The long-term consequences of untreated cavities in mouth can be severe. Beyond intense pain, an untreated cavity can lead to:
- Tooth Loss: The tooth may become so damaged it cannot be saved and must be extracted.
- Spread of Infection: An abscess can cause a serious infection that spreads to the jaw, head, or neck. In rare cases, it can be life-threatening.
- Chewing Problems: Painful or missing teeth hinder chewing, which can affect nutrition.
- Alignment Issues: A lost tooth can cause other teeth to shift, affecting your bite and leading to more dental issues.
A painful cavity means decay has reached the tooth’s deeper layers, but it’s not too late. Prompt dental care can often save the tooth and prevent further complications. For more information on advanced cavities and their potential impact, refer to this resource from Cleveland Clinic.
How Dentists Diagnose and Treat Cavities
At Casey Dental, we prioritize prevention. But if a cavity in mouth does develop, early diagnosis is key to minimally invasive treatment. We use several techniques to detect them:
- Visual Examination: We look for visual signs of decay like white spots, discoloration, or holes during your check-up.
- Dental Explorer (Probe): We use this tool to feel for soft or sticky spots on tooth surfaces that indicate decay.
- Dental X-rays: X-rays are essential for finding hidden decay between teeth or under fillings, showing us the extent of the damage.
- Dye Detection and Laser Fluorescence: We may use special dyes or lasers to find very early or hidden decay.
Regular dental exams are key to prevention, allowing us to catch problems when they are small and easy to treat. You can learn more about the importance of Regular Dental Examinations on our website.
Early Stage Treatment: Reversing the Damage
The good news is that the earliest stage of decay (a white spot on the enamel) is often reversible. This process, called remineralization, relies on fluoride and good oral hygiene.
- Fluoride Treatments: Professional, high-concentration fluoride gels or varnishes strengthen enamel, making it more acid-resistant and helping it repair itself.
- Fluoride Toothpaste: Brushing twice daily with fluoride toothpaste provides continuous protection and aids remineralization.
- Dietary Changes: Limiting sugary and acidic foods gives teeth a break from acid attacks, allowing them to rebuild.
- Improved Oral Hygiene: Proper brushing and flossing remove plaque, the source of acid.
Fluoride integrates into the enamel, making it harder and more acid-resistant. It also attracts minerals from saliva to repair early decay. This means an early cavity can sometimes heal without a filling!
Restorative Treatments for Cavities in Mouth
Once a hole forms, a cavity in mouth is permanent and requires restorative treatment. We remove the decay and restore the tooth’s structure. The treatment depends on the cavity’s size and depth:
- Dental Fillings: This is the standard treatment for most cavities. We remove the decay, clean the area, and fill the space. At Casey Dental, we use tooth-colored fillings for a natural look. You can learn more about Dental Fillings and what tooth fillings are made of on our site.
- Crowns: For extensive decay that weakens the tooth, a crown (or cap) is used. It covers the entire tooth, providing strength and protection.
- Root Canals: If decay reaches the tooth’s inner pulp, a root canal is needed to treat the infection and pain. We remove the infected pulp, clean and seal the tooth, and usually place a crown for protection.
- Tooth Extraction: This is a last resort when a tooth is too damaged to be saved. Removing it may be necessary to protect your overall oral health.
Pain indicates that decay has reached deeper layers, but it rarely means it’s too late. Prompt treatment can almost always repair the cavity and save the tooth. Don’t hesitate to reach out if you’re experiencing pain.
Your Ultimate Guide to Cavity Prevention
We believe that prevention is always the best medicine, especially when it comes to cavities in mouth. Why treat a problem when we can stop it from happening in the first place? The statistics are compelling: dental sealants on the back teeth prevent 80% of cavities, and children who drink fluoridated tap water have fewer cavities. These are powerful tools in our arsenal against tooth decay.
At-Home Oral Hygiene
Our daily habits at home form the frontline defense against cavities. Consistent and proper oral hygiene is non-negotiable:
- Brushing Twice Daily: We recommend brushing your teeth at least twice a day, especially before bed and after breakfast, using a soft-bristled toothbrush and fluoride toothpaste. Proper technique is crucial – make sure to gently brush all surfaces of your teeth, including the outer, inner, and chewing surfaces, for at least two minutes each time.
- Flossing Daily: Brushing alone isn’t enough. Flossing daily removes food particles and plaque from between your teeth and under the gumline, areas your toothbrush can’t reach. This is where many cavities often start.
- Using Fluoride Toothpaste: Fluoride toothpaste is your everyday superhero. It helps strengthen your tooth enamel, making it more resistant to acid attacks, and aids in the remineralization of early decay.
- Rinsing with Water After Meals: A quick rinse with water after snacks or meals, especially after consuming sugary or acidic items, can help wash away food debris and neutralize some of the acids, giving your teeth a chance to recover.
For more valuable insights and specific tips on maintaining excellent oral health as an adult, the CDC provides helpful Tips for adult oral health.
Professional Dental Care and Treatments
While at-home care is vital, it needs to be complemented by professional dental care. Your regular visits to Casey Dental are essential for comprehensive cavity prevention and early detection.
- Regular Dental Cleanings: We recommend scheduling professional dental cleanings every six months. Even the most diligent brushers and flossers can miss spots where plaque and tartar build up. Our skilled hygienists remove this stubborn buildup, polish your teeth, and give you that incredibly clean feeling. These cleanings are critical for preventing cavities and gum disease. You can learn more about the importance of regular dental cleaning on our website.
- Professional Fluoride Applications: During your visits, we may apply professional-strength fluoride treatments (gels or varnishes), especially if you or your child are at higher risk for cavities. These treatments provide a concentrated dose of fluoride that significantly strengthens tooth enamel.
- Dental Sealants Explained: Dental sealants are a fantastic preventive measure, particularly for children and teenagers, but adults can benefit too. They are thin, plastic coatings that we paint onto the chewing surfaces of your back teeth (molars). These surfaces often have deep pits and grooves where food particles and bacteria can easily get trapped, making them prime spots for cavities. The sealant acts as a protective barrier, “sealing out” the food and bacteria and preventing decay. Sealants are quick to apply, painless, and can last for several years.
Frequently Asked Questions about Cavities
Here are answers to common questions we hear about cavities in mouth from our patients in Pittston and across Luzerne County, PA:
Are cavities contagious?
While you can’t “catch” a cavity like a cold, the bacteria that cause them (Streptococcus mutans) are contagious. They can be transmitted through saliva by sharing utensils, cups, or kissing. This is why parents can pass these bacteria to their infants, increasing the child’s cavity risk. The bacteria are contagious, not the cavity itself.
How do cavities affect older adults?
Older adults face a higher risk of developing cavities in mouth, especially on tooth roots, due to unique challenges.
- Receding Gums: Gums often recede with age, exposing tooth roots. Roots are covered by cementum, which is softer than enamel and decays more easily, leading to hard-to-treat root cavities.
- Dry Mouth (Xerostomia): Many medications common among older adults cause dry mouth. Reduced saliva flow is a major risk factor for cavities, as saliva is needed to neutralize acid and repair enamel.
- Existing Dental Work: Old fillings and crowns can wear down or crack, creating hiding spots for bacteria that cause decay.
Statistics show the risk: 96% of adults 65+ have had a cavity. However, thanks to improved dental care, most adults keep their teeth for life. Regular check-ups and consistent hygiene are crucial for older adults to maintain their natural teeth.
You can find more helpful advice for maintaining a healthy smile later in life with these oral health tips for older Americans.
Conclusion
We hope this guide has demystified cavities in mouth and empowered you with the knowledge to protect your oral health. While cavities are incredibly common, they are largely preventable. The power to maintain a healthy, beautiful smile lies in your hands through consistent good oral hygiene and mindful dietary choices.
Your partnership with a trusted dental professional is invaluable. Regular check-ups, professional cleanings, and early intervention are key to a lifetime of healthy teeth. At Casey Dental, we are committed to providing comprehensive Family Dentistry services to our community in Pittston, Scranton, and throughout Luzerne County, PA. We’re here to support you and your family with personalized care, utilizing cutting-edge technology to ensure your comfort and optimal oral health.
Don’t wait for pain to be your guide. Take control of your oral health today! We invite you to learn more about dental cavities and the importance of dental care and schedule your next appointment with us. Let’s work together to keep your smile bright and cavity-free!


